Eating Disorder Rehab Admissions Process
Deciding to seek treatment can be difficult, but reaching out for help and navigating the admissions criteria for eating disorder rehab shouldn’t be. Finding the proper care is essential if you’re worried about your health or that of someone you love. We’re here to assist you. Keep reading for everything you need to know about the eating disorder admissions process.
How To Get Into Rehab for Eating Disorders Treatment
The eating disorder admission requirements can vary from center to center. However, below is a step-by-step outline that you can generally apply:
- Inquire about admission to the eating disorder rehab facility.
- Undergo an assessment to evaluate your needs.
- Verify insurance coverage for eating disorder treatment.
- Discuss the treatment plan and financial arrangements.
- Complete admission paperwork and necessary preparations.
- Be admitted to the facility and receive orientation.
- Start the treatment process under the guidance of the treatment team.
Treatment programs for eating disorders vary and may include outpatient and inpatient options. The type of program that’s best for you depends on the severity of your disorder and your overall health. Both types of programs typically offer a combination of individual therapy, group counseling, and skills training. Inpatient programs offer more intensive care, including medical monitoring and supervision, while outpatient programs allow you to live at home and continue with certain everyday activities. Your treatment team will work with you to develop a personalized plan that fits your needs and promotes recovery.
Get Admitted Into Rehab With Us
Get immediate treatment help now. 100% safe & confidential.
CALL (866)-461-3339
Contact us to schedule a free confidential assessment with a licensed clinician.
Eating Disorders Rehab Admissions Form
Complete the eating disorders rehab admissions form below to receive a prompt call back from a member of our experienced and compassionate admissions staff. With the eating disorder rehab intake form serving as the initial point of contact, it allows us to promptly reach out to you and guide you through the next steps of admission, including verifying insurance coverage, scheduling an assessment, and addressing any questions or concerns you may have. Our goal is to provide a seamless and supportive experience from the moment you complete the admissions form to your successful entry into our rehab program. Start your journey to recovery today by completing the admissions form below and taking the first step towards a healthier and happier life.
What is an Eating Disorder?
Eating disorders are medical conditions that significantly impact a person’s eating habits, thoughts, and emotions. While most people have occasional concerns about their health, weight, or appearance, some develop an unhealthy fixation on weight loss, body shape, and controlling their food intake, resulting in an eating disorder.
Eating disorders can cause significant harm to both physical and mental health and, in some cases, can even be life-threatening. These disorders often occur alongside other conditions, such as mood and anxiety disorders, obsessive-compulsive disorder, and alcohol and substance use disorders.
The causes of eating disorders are not fully understood. Still, like other mental health conditions, there are potentially multiple factors that can vary from person to person and contribute to their development:
- Individuals may possess genes that heighten their susceptibility to developing eating disorders.
- Eating disorders may be influenced by biological factors, such as alterations in brain chemicals.
In addition, there are specific factors that can raise the likelihood of developing an eating disorder, including the following:
- Family history. Individuals with a family history of eating disorders are at a higher risk of developing an eating disorder themselves. While genes and hereditary factors may increase the risk of developing an eating disorder, the condition can also affect people with no family history of the condition.
- Other mental health issues. Experiencing trauma, anxiety, depression, obsessive-compulsive disorder, and other mental health problems can elevate the risk of developing an eating disorder.
- Dieting and starvation. Repeatedly going on diets can increase the likelihood of developing an eating disorder. This is particularly true when one’s weight fluctuates due to constantly starting and stopping new diets.
Research shows that many symptoms of eating disorders are symptoms of starvation. Starvation can negatively affect the brain and lead to changes in mood, rigid thinking, anxiety, and a reduced appetite. These effects may contribute to ongoing unhealthy eating patterns, making it harder to adopt healthy habits again.
- A history of weight bullying. Individuals who have experienced teasing or bullying related to their weight are at a higher risk of developing eating disorders and other eating-related issues. This encompasses those who have felt shame about their weight due to peers, healthcare providers, coaches, teachers, or family members.
- Life changes, such as going to college, moving, starting a new job, or experiencing family or relationship problems, can cause stress. This stress can potentially increase the likelihood of developing an eating disorder.
What is an Eating Disorder Rehab Center?
An eating disorder rehab center, or an eating disorder treatment center or facility, is a specialized facility providing comprehensive and intensive care for individuals struggling with eating disorders. These centers offer a structured and supportive environment where you or your loved one can receive professional treatment, therapy, and guidance to address eating disorders and related mental health issues.
The primary goal of an eating disorder rehab center is to help you regain a healthy relationship with food, your body, and yourself. Treatment approaches may include medical supervision, nutritional counseling, individual and group therapy, psychiatric support, and various evidence-based therapies tailored to your needs. The length of stay in an eating disorder rehab center can vary depending on the severity of the disorder and your treatment progress.

What are the Different Types of Eating Disorders?
There are various types of eating disorders, each with its own symptoms and diagnostic criteria. However, all of these conditions share a common characteristic – an intense preoccupation with food, eating, and, in some cases, weight. Below are the descriptions and symptoms associated with the most common eating disorders.
Anorexia Nervosa
Anorexia nervosa is a serious condition that involves self-starvation and weight loss, which results in a significantly low weight for the individual's height and age. It has one of the highest mortality rates among psychiatric diagnoses, second only to opioid use disorder. Typically, an adult with anorexia nervosa will have a body mass index (BMI) under 18.5.
The dieting behavior associated with anorexia nervosa is often driven by an intense fear of gaining weight or becoming fat. Even if individuals with anorexia claim they want to gain weight, their actions often contradict their words. For example, they may only consume small amounts of low-calorie foods and excessively exercise.
Anorexia nervosa has two subtypes:
- Restricting type: Losing weight primarily by dieting, fasting, or excessively exercising
- Binge-eating/purging type: Engaging in intermittent binge eating and/or purging behaviors
As time goes on, a few of the below symptoms or a combination of these may arise due to behaviors of starving oneself or purging:
- Menstrual periods stop
- Dizziness or fainting (caused by dehydration)
- Weak and brittle hair/nails
- Intolerance to cold
- Muscle weakness/wasting
- Heartburn and acid reflux (in those who vomit)
- Severe constipation, bloating, and fullness after meals
- Stress fractures from compulsive exercise
- Bone loss resulting in osteopenia or osteoporosis (bone thinning)
- Depression
- Irritability
- Anxiety
- Poor concentration
- Fatigue
Anorexia nervosa can lead to serious health issues that can be life-threatening, such as heart rhythm abnormalities, kidney problems, or seizures, especially in those who vomit or use laxatives.
A nutritional plan helps patients counter anxiety about eating and practice consuming various foods of different calorie densities across regularly spaced meals. The most effective treatment for adolescents and emerging adults involves helping parents support and monitor their child's meals. Addressing body dissatisfaction is also important, even though it frequently takes longer to improve than weight and eating habits.
If outpatient treatment is ineffective for severe anorexia nervosa, admission to an inpatient or residential behavioral specialty program may be necessary. Most specialty programs are effective with weight gain and establishing healthy eating habits. However, with all conditions of this severity, there is still a risk of relapse in the first year following program discharge.
Bulimia Nervosa
Alternating between dieting or consuming only low-calorie "safe foods" and bingeing on "forbidden" high-calorie foods is a common feature of this eating disorder. "Binge eating" refers to consuming a lot of food quickly and feeling like you have no control over what or how much you consume.
The habit of binge eating is typically secretive and accompanied by emotions of guilt or embarrassment. Binge eating can involve consuming massive amounts of food quickly and past fullness, causing nausea and discomfort. They may occur weekly, typically followed by "compensatory behaviors" to prevent weight gain, including fasting, vomiting, laxative misuse, or compulsive exercise.
Individuals with bulimia nervosa are excessively preoccupied with thoughts of food, weight, or shape, which can negatively impact their self-worth. Unlike anorexia nervosa, people with bulimia nervosa may be underweight, average-weight, overweight, or even obese. However, instead of having bulimia nervosa, individuals are thought to have anorexia nervosa binge-eating/purging type if they are substantially underweight.
It can be challenging to identify if someone has bulimia nervosa because they may not appear underweight, and their behaviors are often hidden and go unnoticed. Below are some typical signs that someone may be struggling with bulimia nervosa:
- Frequent bathroom visits directly after meals
- Excessive amounts of food disappearing or unexplained empty wrappers and containers
- Chronic sore throat
- Dehydration
- Swelling in the cheeks
- Dental decay
- Heartburn and gastroesophageal reflux
- Misuse of laxatives or diet pills
- Recurring or unexplained diarrhea
- Feeling dizzy
- Fainting from excessive purging behaviors
Bulimia nervosa can have serious and life-threatening consequences like esophageal tears, gastric rupture, and cardiac arrhythmias. It's crucial to have medical monitoring for severe cases of the disorder to identify and treat any potential complications.
The most effective treatment for bulimia nervosa is outpatient cognitive behavioral therapy (CBT). This therapy helps patients establish healthy eating habits and manage thoughts and emotions to break free from the disorder.
Antidepressants like fluoxetine can also reduce the urge to binge and vomit. For young people with bulimia nervosa, eating disorder-focused family-based treatment that teaches caregivers how to help their loved ones establish healthy eating habits may also be effective.
Binge Eating Disorder
Binge eating disorder is characterized by consuming large amounts of food in a short time, causing loss of control and distress. Unlike bulimia, individuals do not engage in compensatory behaviors. This disorder can lead to obesity and other serious health issues.
To diagnose binge eating disorder, one must have frequent episodes of overeating (at least once a week for three months) accompanied by a feeling of loss of control and three or more of the following characteristics:
- Eats more rapidly than normal
- Eats until uncomfortably full
- Consumes excessive amounts of food when not hungry
- Eats alone due to feeling embarrassed
- Feels disgusted with oneself, depressed, or very guilty after binging
Individual or group-based CBT is the most effective treatment for binge eating disorder, similar to bulimia nervosa. Interpersonal therapy (IPT) can also be helpful.
Pica
Pica involves repeatedly consuming non-food items with no nutritional value. This behavior must persist for at least one month and be severe enough to require clinical attention. The substances ingested may vary based on age and availability and include items such as paper, paint chips, cloth, hair, clay, chalk, metal, pebbles, soap, charcoal, or string.
Individuals with pica typically don’t have an aversion to food in general, and the behavior is inappropriate for their developmental level or culturally supported practices. Pica can first occur in childhood, adolescence, or adulthood but is most common in childhood. It is not diagnosed in children under 2, as putting small objects in their mouths is a normal part of development at this age.
The condition is often associated with autism spectrum disorder (ASD) and intellectual disability but may also occur in normally developing children. Those diagnosed with pica are at risk for intestinal blockages or toxic effects from the substances consumed, such as lead in paint chips.
Treatment for pica involves identifying and addressing any nutritional deficiencies and behavior interventions to redirect the individual from non-food items and reward them for avoiding such items.
Rumination Disorder
Rumination disorder is when swallowed food is brought back into the mouth and re-chewed and swallowed again or spat out. This can happen in infancy, childhood, adolescence, or adulthood. Rumination can occur in other mental disorders. However, the severity must be significant enough to require separate clinical attention to make a diagnosis.
To meet the diagnostic criteria for rumination disorder, the behavior must:
- Occur repeatedly in a minimum of 1 month
- Not be caused by a gastrointestinal or medical issue
Take place independently of any other behavioral eating problems
Avoidant/Restrictive Food Intake Disorder (ARFID)
ARFID, a recently identified eating disorder, is characterized by eating disturbances that repeatedly fail to fulfill nutritional requirements. ARFID doesn't entail limiting food intake because of factors like food shortage, frequent dieting, cultural customs (like fasting), or typical behaviors seen in young children who are picky about what they eat.
If someone has ARFID, their avoidance or limited range of food choices may be caused by one or more of the following reasons.:
- Poor appetite and lack of interest in eating or food
- Complete avoidance of some foods due to their sensory qualities, such as their texture, look, color, and smell
- Extreme anxiety or concern due to the fear of negative consequences like choking, nausea, vomiting, constipation, or an allergic reaction. This disorder may develop as a response to a traumatic event, like a choking episode or food poisoning, leading to a gradual avoidance of more foods
To diagnose ARFID, there must be difficulties with eating that are linked to one or more of the following:
- Significant and noticeable weight loss (or failure to achieve expected weight gain in children)
- Extreme nutritional deficiency
- Reliance on a feeding tube or oral nutritional supplements to maintain healthy nutrition intake
- Interference with social functioning (i.e., inability to eat with others)
People with ARFID may experience physical and psychological health issues similar to those seen in individuals with anorexia nervosa, as well as malnutrition. However, ARFID differs from anorexia nervosa as it is not driven by concerns about body weight or shape.
Avoiding or restricting certain foods is often developed in infancy or early childhood and can persist into adulthood, although it can also begin at any point in life. This condition can cause increased stress during mealtimes and social eating situations for the individual and their family.
Treatment for ARFID involves a personalized plan that may require the involvement of specialists, such as a mental health professional or registered dietitian nutritionist.
Other Specified Feeding and Eating Disorders (OSFED)
This category of diagnoses covers eating disorders or behaviors that cause distress and affect social, family, or work life but do not fit into other established categories. This may be because the frequency of the behavior does not meet the diagnostic criteria, such as in bulimia or binge eating disorder, or because the weight criteria for diagnosing anorexia nervosa are not met.
An example of this type of diagnosis is "atypical anorexia nervosa." This includes people with anorexia nervosa-like behaviors and concerns about their weight or appearance, who, while having an above-average starting weight, are not regarded to be underweight by their BMI.
Individuals with atypical anorexia nervosa who experience rapid weight loss through extreme weight control behaviors may be at high risk for medical complications, despite appearing to be at a normal or above-average weight. The speed of weight loss is a significant factor in developing medical complications.
Does My Insurance Cover Rehab Eating Disorder Treatment?
Rehab insurance coverage for eating disorder treatment varies depending on your policy, the treatment facility, and the level of care needed. Keep in mind that in-network providers will provide more comprehensive coverage, and be aware of limitations, deductibles, co-pays, and co-insurance. Additionally, pre-authorization and demonstrating medical necessity may be required.
Call 866-461-3339 now to review the specifics of your insurance coverage for eating disorder treatment.
More Questions About Getting Admitted Into Inpatient Rehabilitation Treatment?
Call Now on 866-461-3339
Alternatively, you can fill up the rehabilitation admissions form and and a member of our team will get in touch with you.
How to Find Eating Disorder Rehabilitation Centers Near Me
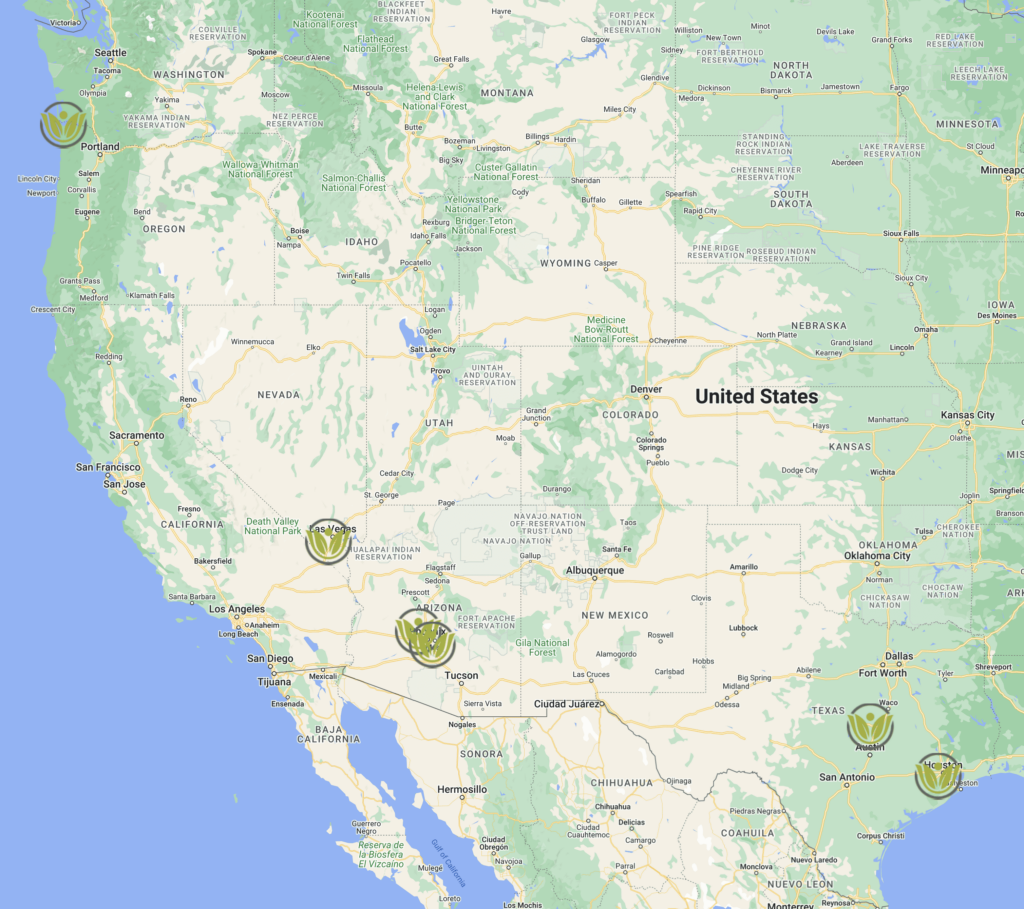
At Virtue Recovery Center, we believe that "all foods fit" when it comes to our nutritional philosophy. This forms the basis of our dietary program, which includes and supports individuals of all shapes and sizes. We specialize in treating eating disorders by promoting mind-body connection through compassion, education, and shame reduction.
We offer personalized care beginning with a convenient and free assessment. Just call 866-461-3339. You are also welcome to visit one of our nationally accredited treatment facilities outlined below:
Recovery Centers in Arizona
- Chandler, Arizona: 111 S Hearthstone Way, Chandler, AZ 85226, United States
- Sun City West, Arizona: 13951 W Meeker Blvd, Sun City West, AZ 85375, United States
Recovery Centers in Texas
- Houston, Texas: 9714 S Gessner Rd, Houston, TX 77071, United States
- Killeen, Texas: 5200 S W S Young Dr, Killeen, TX 76542, United States
Recovery Centers in Nevada
- Las Vegas, Nevada: 8225 W Robindale Rd, Las Vegas, NV 89113
Recovery Centers in Oregon
- Astoria, Oregon: 263 W Exchange St, Astoria, OR 97103, United States
Alternative Ways To Find Nearby Rehabilitation Centers
- Research Online: Conduct an online search using keywords such as "eating disorder inpatient rehab within my vicinity" or “eating disorder treatment close to me,” followed by your exact location.
- Use Treatment Referral Helplines: You can contact referral helplines, hotlines, or support organizations such as the Substance Abuse and Mental Health Services Administration (SAMHSA). They can provide a list of the nearest reputable eating disorder treatment centers. Additionally, they can guide you in close-by treatment programs that suit your specific needs.
- Consult with Local Healthcare Professionals: Connect with professionals in your immediate area specializing in eating disorder treatment. They can offer helpful recommendations and insights about conveniently located programs.
- Seek Recommendations: Ask for recommendations from anyone you know who has undergone an eating disorder rehab assessment process. Their personal experiences can help you identify reputable rehab centers within reach.
- Check Online Reviews and Testimonials: To assess the quality of care and effectiveness of treatment, read online reviews and testimonials. Concentrate on feedback regarding treatment programs, staff, amenities, and overall satisfaction.
- Verify Licensing and Accreditation: Before choosing a rehab center, make sure it is licensed and accredited by regulatory bodies that ensure compliance with quality standards and ethical practices.
- Consider Location and Accessibility: Considering factors such as proximity to your home, work, or support network will ease some of the challenges associated with the eating disorder admissions process. Do you prefer a more localized facility, or are you open to traveling further?
- Assess Treatment Approaches and Services: Research the treatment options and services, including therapies, amenities, and ongoing support. Ensuring a facility’s offerings meet your specific needs and preferences is crucial.
- Contact the Rehab Centers: Be sure to ask about the specific programs offered, the treatment philosophy, the staff qualifications, the amenities available, and any personal preferences or requirements you may have. It's also important to inquire about the availability of customized treatment plans.
- Verify Insurance Coverage and Cost: Check if a program accepts your insurance or offers financing options before committing. Inquire about the program's total cost, including additional expenses, to ensure that it aligns with your budget and available resources.
- Visit the Facility: If possible, visit the eating disorder treatment centers you're interested in. This will allow you to see the facility, meet the staff, and get a feel for the treatment environment. Moreover, it’s the perfect opportunity to ask questions.
What Does Eating Disorder Rehabilitation Admissions or Intake Mean?
Eating disorder rehabilitation admissions or intake refers to the process by which you enter and begin receiving treatment at an eating disorder rehab center. It is the initial step you’ll take to access the care and support needed for an eating disorder.
During the admissions or eating disorder treatment intake, you’ll typically be evaluated by a team of professionals, including doctors, therapists, and other specialists, to assess your eating disorder’s severity and determine the most appropriate treatment plan. This evaluation often includes a thorough physical examination, a psychological assessment, and a discussion of your medical history, eating behaviors, and related concerns.
The information gathered during the intake helps the treatment team develop an individualized treatment plan that addresses your specific needs and challenges. It is also an opportunity to ask questions, express your goals and concerns, and understand what to expect during your stay at the rehabilitation center.
What is the Eating Disorder Inpatient Rehab Admissions and Intake Process?
The eating disorder inpatient rehab admissions and intake process refers specifically to the steps to enroll in an eating disorder rehab program. The specific details surrounding the eating disorder inpatient admission criteria and intake process can vary between treatment centers. However, below is a general overview of what the process may involve:
- Initial inquiry: You can typically reach out to the rehabilitation center you’re interested in by phone, email, or an online form.
- Pre-assessment: The treatment facility may begin by assessing suitability for eating disorder rehab over the phone or through a questionnaire to gather initial information about your medical history, eating disorder symptoms, mental health concerns, and other relevant details.
- Clinical assessment: Once serious interest in admission is expressed and you’ve satisfied the eating disorder admission criteria, you may be invited for an in-person or virtual clinical assessment. This involves meeting with healthcare professionals specializing in eating disorder treatment. The assessment helps determine the severity of the eating disorder, any co-occurring conditions, and the appropriate level of care.
- Medical evaluation: A thorough medical evaluation assesses your physical health, including vital signs, laboratory tests, and potential medical complications related to the eating disorder.
- Treatment planning: A customized treatment plan is developed based on the information gathered during the assessment and evaluation stages. This plan outlines the specific interventions, therapies, and goals guiding your treatment.
- Insurance and financial arrangements: The rehab center will discuss insurance coverage, financial responsibilities, and any necessary paperwork with you.
- Admission: You’ll officially be admitted to the eating disorder inpatient rehab center once intake procedures for eating disorder recovery are completed and if it is determined that inpatient treatment is appropriate. You’ll be provided with information about what to bring, the rules and guidelines of the facility, and any other relevant details.
What is the Eating Disorder Outpatient Rehab Admissions and Intake Process?
The specific details and steps involved in the eating disorder outpatient rehab admissions and intake process can vary between treatment centers. Additionally, the assessment and intake process for eating disorder recovery in an outpatient setting is similar to that of an inpatient. Below are the notable similarities and differences:
Similarities:
- Initial inquiry: Inpatient and outpatient rehab programs typically start with an initial inquiry where you or your loved one expresses interest in seeking treatment.
- Clinical assessment: Both programs involve a clinical assessment conducted by a team of healthcare professionals. This assessment helps determine the severity of the eating disorder, identify any co-occurring conditions, and guide treatment planning.
- Treatment planning: Both develop a customized treatment plan based on the information gathered during the assessment. The plan outlines the specific interventions, therapies, and goals for treatment.
- Insurance and financial arrangements: Both programs discuss insurance coverage, financial responsibilities, and necessary paperwork.
Differences:
- Level of care: The main difference between inpatient and outpatient rehab is the intensity of care provided. Inpatient rehab means staying at the facility full-time for a designated period. Outpatient rehab, on the other hand, offers treatment sessions part-time so you can still live at home and take care of your daily responsibilities.
- Medical evaluation: Inpatient care typically involves a more thorough medical evaluation to account for the higher severity level and potential health complications associated with residential treatment. Outpatient rehab may offer a briefer medical assessment or refer you to external healthcare providers for medical evaluations.
- Program orientation: Inpatient programs typically include a program orientation where you’re provided with detailed information about the facility, rules, expectations, and daily routines. Outpatient programs may have a more streamlined orientation process since you won’t reside at the facility.
- Treatment intensity and duration: Inpatient rehab offers round-the-clock care and a highly structured environment for intensive treatment. The duration of inpatient rehab can vary but is typically longer than outpatient programs. Outpatient rehab provides treatment sessions on a part-time basis, with varying levels of intensity and duration depending on the program and your unique needs.
What is the Initial Intake Assessment Process for Eating Disorder Treatment?
The initial eating disorder rehab intake assessment process for treatment typically involves several steps to gather comprehensive information about your medical history, eating disorder symptoms, mental health status, and other relevant details. While the specific procedures may vary between treatment centers, they usually include a psychological and nutritional assessment, among other aspects.
The process is crucial to understanding your individualized needs, tailoring the treatment plan, and determining the appropriate level of care. It helps the treatment team provide comprehensive, customized care throughout your recovery. Call 866-461-3339 to schedule your free assessment.
Are There Ongoing Evaluations During the Eating Disorder Recovery Process?
Yes, ongoing evaluations are an essential part of the eating disorder recovery process. Regular assessments and evaluations are conducted throughout the treatment and recovery journey to monitor progress, adjust treatment plans as needed, and ensure your overall well-being. These evaluations may take various forms and involve multiple healthcare professionals, including therapists, medical providers, and dietitians.
Ongoing evaluations ensure that the treatment approach remains effective and you receive the necessary support throughout your eating disorder recovery process. They also provide opportunities to address emerging challenges, celebrate milestones, and make informed decisions to optimize your overall health toward long-term recovery.
How Do I Get Admitted to Eating Disorder Rehab?
The eating disorder admission requirements can vary from center to center. However, below is a step-by-step outline that you can generally apply:
- Inquire about admission to the eating disorder rehab facility.
- Undergo an assessment to evaluate your needs.
- Verify insurance coverage for eating disorder treatment.
- Discuss the treatment plan and financial arrangements.
- Complete admission paperwork and necessary preparations.
- Be admitted to the facility and receive orientation.
- Start the treatment process under the guidance of the treatment team.
How to Find Eating Disorder Rehabilitation Centers Near Me
At Virtue Recovery Center, we believe that “all foods fit” when it comes to our nutritional philosophy. This forms the basis of our dietary program, which includes and supports individuals of all shapes and sizes. We specialize in treating eating disorders by promoting mind-body connection through compassion, education, and shame reduction.
We offer personalized care beginning with a convenient and free assessment. Just call 866-461-3339. You are also welcome to visit one of our nationally accredited treatment facilities outlined below:
- Astoria, Oregon: 263 W Exchange St, Astoria, OR 97103, United States
- Chandler, Arizona: 111 S Hearthstone Way, Chandler, AZ 85226, United States
- Houston, Texas: 9714 S Gessner Rd, Houston, TX 77071, United States
- Killeen, Texas: 5200 S W S Young Dr, Killeen, TX 76542, United States
- Las Vegas, Nevada: 8225 W Robindale Rd, Las Vegas, NV 89113
- Sun City West, Arizona: 13951 W Meeker Blvd, Sun City West, AZ 85375, United States
To find additional eating disorder rehabilitation centers nearby, see below:
- Research Online: Conduct an online search using keywords such as “eating disorder inpatient rehab within my vicinity” or “eating disorder treatment close to me,” followed by your exact location.
- Use Treatment Referral Helplines: You can contact referral helplines, hotlines, or support organizations such as the Substance Abuse and Mental Health Services Administration (SAMHSA). They can provide a list of the nearest reputable eating disorder treatment centers. Additionally, they can guide you in close-by treatment programs that suit your specific needs.
- Consult with Local Healthcare Professionals: Connect with professionals in your immediate area specializing in eating disorder treatment. They can offer helpful recommendations and insights about conveniently located programs.
- Seek Recommendations: Ask for recommendations from anyone you know who has undergone an eating disorder rehab assessment process. Their personal experiences can help you identify reputable rehab centers within reach.
- Check Online Reviews and Testimonials: To assess the quality of care and effectiveness of treatment, read online reviews and testimonials. Concentrate on feedback regarding treatment programs, staff, amenities, and overall satisfaction.
- Verify Licensing and Accreditation: Before choosing a rehab center, make sure it is licensed and accredited by regulatory bodies that ensure compliance with quality standards and ethical practices.
- Consider Location and Accessibility: Considering factors such as proximity to your home, work, or support network will ease some of the challenges associated with the eating disorder admissions process. Do you prefer a more localized facility, or are you open to traveling further?
- Assess Treatment Approaches and Services: Research the treatment options and services, including therapies, amenities, and ongoing support. Ensuring a facility’s offerings meet your specific needs and preferences is crucial.
- Contact the Rehab Centers: Be sure to ask about the specific programs offered, the treatment philosophy, the staff qualifications, the amenities available, and any personal preferences or requirements you may have. It’s also important to inquire about the availability of customized treatment plans.
- Verify Insurance Coverage and Cost: Check if a program accepts your insurance or offers financing options before committing. Inquire about the program’s total cost, including additional expenses, to ensure that it aligns with your budget and available resources.
- Visit the Facility: If possible, visit the eating disorder treatment centers you’re interested in. This will allow you to see the facility, meet the staff, and get a feel for the treatment environment. Moreover, it’s the perfect opportunity to ask questions.
Rehabilitation Treatment Process and Daily Schedule
The eating disorder rehabilitation treatment process and daily schedule can vary between centers. The duration and intensity of therapy sessions and specific services offered may also vary according to your individual needs and the treatment center’s approach. However, below is a general overview of an eating disorder rehabilitation treatment process and daily schedule:
- Assessment: Initial evaluation of your condition, including physical and mental health, to determine an appropriate treatment plan.
- Medical stabilization: If necessary, medical interventions, including medications, are provided to address any immediate health concerns related to the eating disorder.
- Nutritional support: Individualized meal plans and nutritional counseling help restore healthy eating habits and address nutritional deficiencies.
- Therapy sessions: Various forms of therapy are offered, including, but not limited to, the following:[i]
- Individual therapy: One-on-one sessions with a therapist to address underlying issues, develop coping strategies, and promote healing.
- Group therapy: Participating in therapy sessions with peers, led by a therapist, to share experiences, gain support, and learn from others.
- Family therapy: Involving family members to improve communication, foster understanding, and facilitate a supportive environment for recovery.
- Cognitive-Behavioral Therapy (CBT): A therapeutic approach focusing on identifying and modifying unhealthy thoughts and behaviors related to the eating disorder.
- Dialectical Behavior Therapy (DBT): A therapy that combines CBT techniques with mindfulness to promote emotion regulation and effective coping strategies.
- Acceptance and Commitment Therapy (ACT): A therapy that encourages acceptance of difficult emotions while promoting personal values and committed actions towards recovery.
- Body image therapy: Strategies and interventions aimed at improving body image perception and fostering a positive relationship with one’s body.
- Trauma-informed therapy: Addressing any past traumas that may contribute to the development or maintenance of the eating disorder.
- Psychoeducation: Education about eating disorders, nutritional knowledge, relapse prevention, and developing skills to maintain recovery beyond treatment.
- Experiential therapies: Incorporating art therapy, yoga, meditation, equine therapy, and other expressive therapies to enhance self-expression, self-awareness, and relaxation.
- Relapse prevention: Equipping you with strategies and skills to recognize triggers, manage stress, and prevent relapse after leaving the treatment center.
Daily Schedule:
- Mornings: Structured meals and snacks, followed by therapy sessions, including individual or group therapy, nutritional counseling, or psychoeducation.
- Afternoons: Additional therapy sessions, such as body image therapy, trauma-informed therapy, or experiential therapies.
- Evenings: Free time for relaxation, self-reflection, recreational activities, and social interaction with peers in a supportive environment.
Take the first step to recovery
Call 866-611-1628 to speak with a recovery coordinator immediately, or complete the brief form below to receive a prompt call back from a member of our experienced and compassionate admissions staff. All communication is 100% Confidential.
-
Call Anytime
+234706063340 -
Call Anytime
+2348100016873
+2348068327445 -
Send Email
info@dtoindustries.com
dtonig@dtoindustries.com -
Visit Office
12-14 Babs Aminashua, Embassy
Block Surulere Lagos Nigeria
CONTACT
INFORMATION
Some Statistics and Information Specifically about Eating Disorders
- Individuals who have a sibling or parent with an eating disorder have a higher likelihood of developing one themselves.1
- According to experts, differences in brain structure and biology could contribute to developing eating disorders. Specifically, the levels of serotonin and dopamine, which are chemicals that send messages in the brain, may play a role.2
- Binge eating disorder is the most common eating disorder, with a high prevalence among adolescents.3
- According to information gathered from the National Comorbidity Survey Replication (NCS-R) through diagnostic interviews, the average age when a binge eating disorder begins is 21 years old. In comparison, both bulimia nervosa and anorexia nervosa typically start at 18 years old.4
- In the United States, approximately 30 million individuals will experience at least one eating disorder in their lifetime, with an estimated 20 million being women and 10 million being men.5
- Out of all mental illnesses, eating disorders pose the most significant risk of mortality.6
- Eating disorders can impact individuals of all genders, races, and ethnic groups.
- The worldwide prevalence of eating disorders rose from 3.4% to 7.8% between 2000 and 2018.7
- Eating disorders among adolescent females in the United States are the third most prevalent chronic illness.
- A study conducted in 2021 shows that the number of individuals seeking inpatient treatment for an eating disorder doubled from 2018 to 2020.8
- Individuals who identify as a gender different from their assigned sex at birth are more likely to be diagnosed with an eating disorder or report disordered eating habits.9
- According to a study, existing treatments for eating disorders can prevent approximately 42 deaths per 100,000 people under 40 in the United States. The study also suggests that expanding treatment options to more individuals with eating disorders could potentially prevent up to 70.5 deaths per 100,000 people under 40.10
- “Eating Disorders.” NAMI: National Alliance on Mental Illness, www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Eating-Disorders. Accessed 6 July 2023.
- Riva, Giuseppe. “Neurobiology of Anorexia Nervosa: Serotonin Dysfunctions Link Self-Starvation With Body Image Disturbances Through an Impaired Body Memory.” Frontiers in Human Neuroscience, vol. 10, Frontiers Media, Nov. 2016, https://www.frontiersin.org/articles/10.3389/fnhum.2016.00600/full.
- Marzilli, Eleonora, et al. “A Narrative Review of Binge Eating Disorder in Adolescence: Prevalence, Impact, and Psychological Treatment Strategies.” Adolescent Health, Medicine and Therapeutics, vol. Volume 9, Dove Medical Press, Jan. 2018, pp. 17–30. https://doi.org/10.2147/ahmt.s148050.
- Hudson, James I., et al. “The Prevalence and Correlates of Eating Disorders in the National Comorbidity Survey Replication.” Biological Psychiatry, vol. 61, no. 3, Elsevier BV, Feb. 2007, pp. 348–58. https://doi.org/10.1016/j.biopsych.2006.03.040.
- National Eating Disorders Association. “What Are Eating Disorders?” National Eating Disorders Association, 18 Jan. 2023, www.nationaleatingdisorders.org/what-are-eating-disorders.
- “Eating Disorder Facts.” Johns Hopkins All Children’s Hospital, www.hopkinsallchildrens.org/Services/Pediatric-and-Adolescent-Medicine/Adolescent-and-Young-Adult-Specialty-Clinic/Eating-Disorders/Eating-Disorder-Facts. Accessed 6 July 2023.
- SingleCare Team. “Eating Disorder Statistics 2023.” The Checkup, Feb. 2023, www.singlecare.com/blog/news/eating-disorder-statistics.
- Asch, David A., et al. “Trends in US Patients Receiving Care for Eating Disorders and Other Common Behavioral Health Conditions Before and During the COVID-19 Pandemic.” JAMA Network Open, vol. 4, no. 11, American Medical Association, Nov. 2021, p. e2134913. https://doi.org/10.1001/jamanetworkopen.2021.34913.
- Diemer, Elizabeth W., et al. “Beyond the Binary: Differences in Eating Disorder Prevalence by Gender Identity in a Transgender Sample.” Transgender Health, vol. 3, no. 1, Mary Ann Liebert, Inc., May 2018, pp. 17–23. https://doi.org/10.1089/trgh.2017.0043.
- Ward, Zachary J., et al. “Estimation of Eating Disorders Prevalence by Age and Associations With Mortality in a Simulated Nationally Representative US Cohort.” JAMA Network Open, vol. 2, no. 10, American Medical Association, Oct. 2019, p. e1912925. https://doi.org/10.1001/jamanetworkopen.2019.12925.


