How Much Does Rehab Cost with AHCCCS Insurance?
You’ll typically pay part of the cost for covered services through copayments or coinsurance with AHCCCS insurance. These out-of-pocket expenses are based on a sliding scale fee considering your income and other factors. However, the cost of AHCCS rehab coverage can vary according to the specific services received, the duration of treatment, and more.
AHCCCS has different plans and coverage options, and the exact costs associated with rehab services can also vary depending on the specific plan you’re enrolled in. For example, some plans may have more comprehensive coverage with lower out-of-pocket costs, while others may require higher copayments or coinsurance.
You can contact us at 866-461-3339 for detailed information about the specific plan, coverage, and associated costs for rehab services with AHCCCS insurance.
How To Check My AHCCCS Insurance Coverage Levels for Rehab Treatment
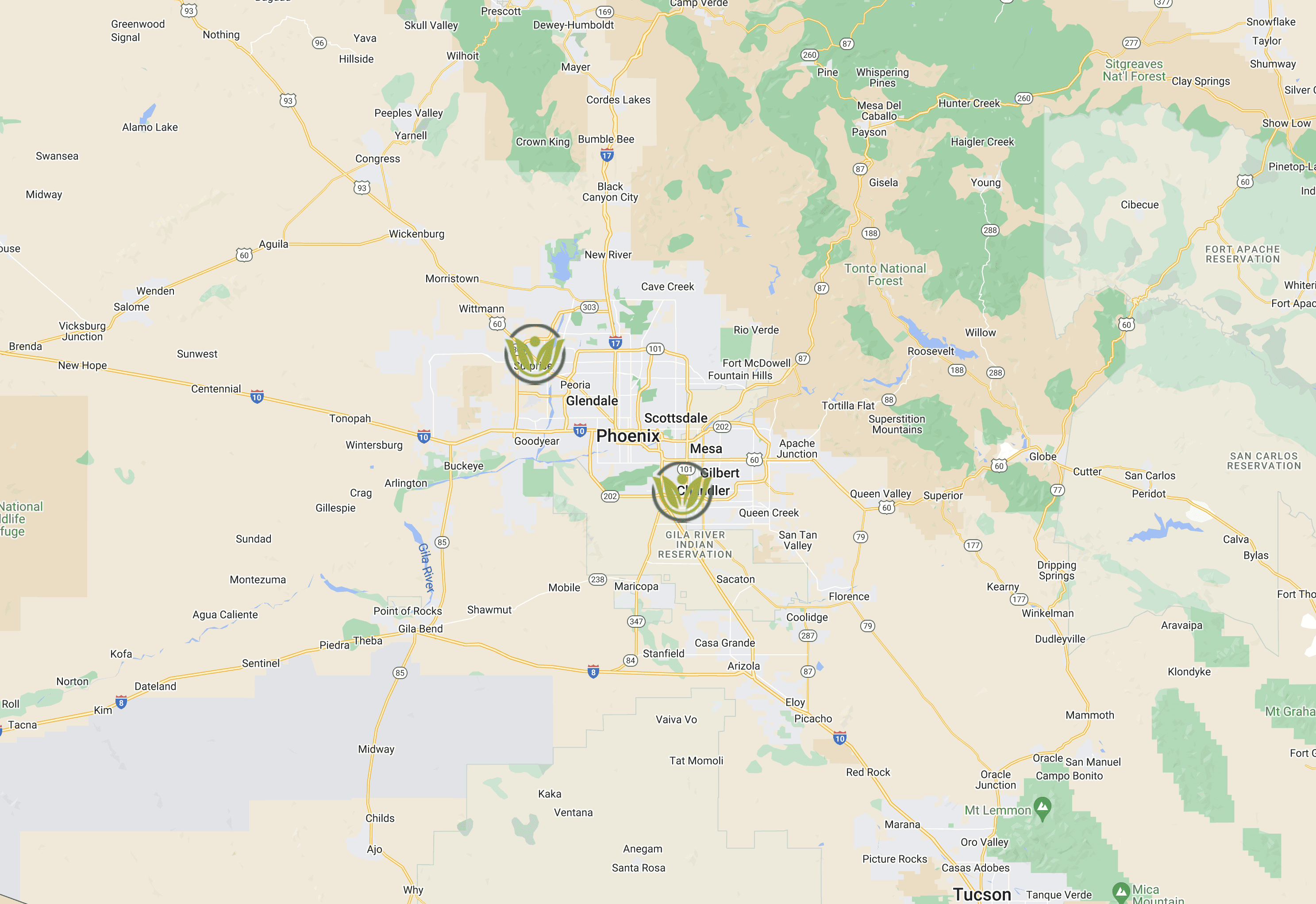
Are you having trouble contacting your insurance provider about your rehab coverage? Virtue Recovery Center can help. Simply fill out our no-obligation online form, and one of our highly qualified staff members will contact your provider to verify your insurance coverage levels. We are in-network with most insurance plans and can answer any questions you may have. Plus, we ensure that all information you provide remains confidential. So, contact us today at 866-461-3339 to discuss your AHCCCS rehab coverage and next steps.
How To Get AHCCCS To Pay for Rehab Treatment
The specific procedures and requirements may vary depending on your circumstances and the AHCCCS plan you are enrolled in. Generally, it begins with ensuring you meet the eligibility requirements for AHCCCS coverage, which are as follows:4
- Residency: You must be a resident of the state of Arizona.
- Citizenship or Immigration Status: You must be a US citizen, US national, or qualified non-citizen with appropriate immigration status.
- Social Security Number: You must provide a valid Social Security number or proof of application for one.
- Income: You must meet income requirements based on household size and income limits set by AHCCCS. Income eligibility varies depending on the AHCCCS program category.
- Categorical Eligibility: You must fall into one of the AHCCCS program categories, such as pregnant women, parents or caretaker relatives, children, adults without dependent children, individuals with disabilities, or individuals aged 65 and older.
- Other Eligibility Factors: Additional factors, such as age, disability status, pregnancy, and household composition, may be considered for eligibility determination.
The above bullet points provide a general overview of eligibility requirements, and there may be specific details and exceptions for each category. For a comprehensive understanding of the eligibility requirements and to determine your eligibility for AHCCCS coverage, call 866-461-3339.
Once you've determined your eligibility, seek a treatment provider. Research and choose a rehab treatment provider or facility that accepts AHCCCS insurance. Contact the provider or facility directly to confirm that they accept your specific AHCCCS plan and to discuss the treatment options available.
You’ll likely need a referral or prior authorization from your primary care provider or the AHCCCS behavioral health service provider to access treatment. Check with your AHCCCS plan or provider to determine if this step is necessary and follow the appropriate procedures.
Once you have obtained the necessary referral or prior authorization, attend the rehab treatment as directed. Ensure you provide your AHCCCS insurance information to the treatment provider or facility. The rehab treatment provider or facility will bill AHCCCS for the covered services. Therefore, ensure they have accurate and up-to-date information regarding your AHCCCS coverage. It's also important to review any Explanation of Benefits (EOB) you receive from AHCCCS to ensure the services are being billed correctly.
Depending on your plan, you may be responsible for copayments or coinsurance for the AHCCCS rehab coverage. Pay any applicable out-of-pocket costs according to the terms of your AHCCCS plan.
Contact AHCCCS directly, consult their official website, or call us at 866-461-3339 for detailed information on accessing and receiving coverage for rehab treatment. Reaching out to your chosen treatment provider or facility can help you navigate insurance proceedings and ensure a smooth payment and reimbursement process.
How Many Times Will AHCCCS Pay for Rehab?
The number of times AHCCCS will pay for rehab depends on the specific circumstances and your treatment needs. AHCCCS rehab coverage is typically determined case-by-case, considering the medical necessity and your treatment progress. AHCCCS will generally cover rehab services as long as they are deemed medically necessary. We will design a treatment planned tailored to your exact needs and work with AHCCCS to make sure you get the required help to continue your journey to recovery,
Rehab Treatment and Insurance Statistics
- Approximately 50% of Arizonans had consumed alcohol in the last month of 2020, and 23% of those people had participated in binge-style drinking. In addition, over 1% reported using methamphetamine the previous year, while 4% reported abusing painkillers.5
- More than 2.4 million Arizonans get physical and behavioral health services from more than 115,000 healthcare professionals via contracted health plans through AHCCCS.
- As of May 1, 2023, 48,528 individuals with a serious mental illness (SMI) were enrolled in AHCCCS.6
- According to the AHCCCS' statistics in its 2018 Annual Report on Drug Abuse Treatment Programs, members who got treatment for a substance use disorder (SUD) improved across the board, but more so in certain areas than others.7
- Over $455 million in service funds was used by AHCCCS for members and families with substance use disorder (SUD) during Arizona’s fiscal year of 2019.8
- Most (55.6%) members enrolled in AHCCCS who received a substance use disorder (SUD) treatment service in2019 were White. In addition, 6.9% of members wereAfrican American, 7.9% were American Indian, 0.6% were Asian, and 0.2% were NativeHawaiian/Pacific Islander. Statewide, 1.7% of members enrolled and served identified asHispanic/Latino.
- Most treated with a substance use disorder (SUD) in 2019 were adults between the ages of 25 and 44, accounting for more than half of all members (53.9%). In addition, 28.7% were between the ages of 45 – 64, and about 3.5%were under 18.
- Methamphetamines were the most common substance used statewide by those in treatment in 2019 at 19.8%, followed closely by opiates at 19.4%. The next substance used was marijuana at 19.0%, followed by alcohol at 18.8%. The least common substance reported was other sedatives/tranquilizers and inhalants (0.2%).
- 183,039 AHCCCS members with a substance use disorder (SUD) were treated in 20219
- The total expenditures for inpatient psychiatric treatment in 2022 for AHCCCS members 21+ was $174,659,408.70.10